Gastric Feed Information
Gastric Feed Articles:
- The Use of Blenderized Tube Feeding in Pediatric Patients
- Blenderized Tube Feeding: Suggested Guidelines to Clinicians
- Maintaining hydration in enteral tube feeding
- History of Enteral Nutrition Therapy
In writing this section, I consulted with Laura Schoenfeld, MPH, RD, a Registered Dietitian with a Masters in Public Health Nutrition (MPH) who has a strong background in functional medicine. For Laura’s Master’s thesis, in 2013 she published a paper entitled “The Use of Blenderized Tube Feeding in Pediatric Patients: Evidence and Guidelines for Dietetic Practice.” I also consulted with Kathryn Hayes CCC-SLP, Katy Haldiman RN (The Paleo Nurse), and Jeremy Lampel, MS, RD, CDE, a registered dietitian and certified diabetes educator with a Master’s degree in nutritional science. In December of 2014, Practical Gastroenterology published an article titled “Blenderized Tube Feeding: Suggested Guidelines to Clinicians.”
The Blenderized Tube Feeding: Suggested Guidelines to Clinicians article mentioned above states:
“…the best candidate is a patient and/or caregiver who made the decision to ‘try’ this feeding option, and is willing to commit their time and effort for instruction and preparation of BTF [Blenderized Tube Feed].”
The article above explains how a supporter who is willing to commit the time can work with those who are on the patient’s healthcare team (i.e. nurses, dietitians, and SLPs) to feed a patient in this manner.433 Soon after an injury is a vulnerable period in which nutrition is vitally important. This importance is unfortunately often overlooked.
_____________________________________________________
Gastric Feed Considerations for Clinicians
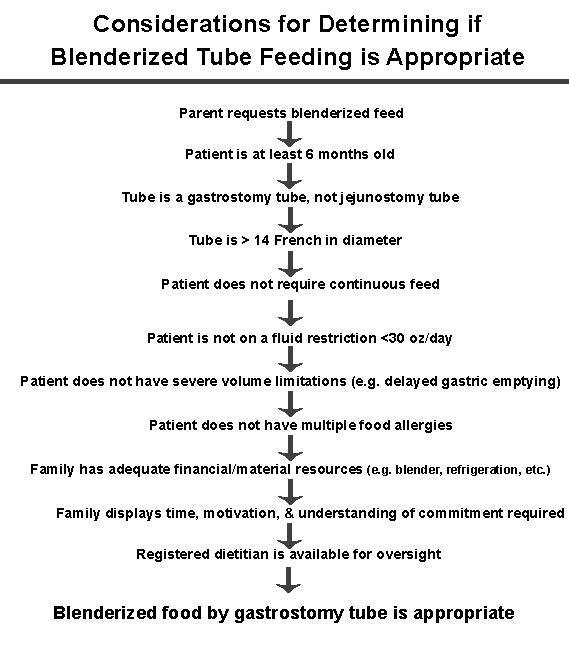
The chart below is adapted from the article written by Laura Schoenfeld, MPH, RD concerning blenderized tube feeding in pediatric patients. It details step-by-step considerations for determining if blenderized tube feeding is appropriate for a patient. In it, if we change the word “parent“ to “patient or caregiver,” the same criteria apply to patients of any age. This is a list of the minimum criteria for clinicians to consider before switching to a blenderized tube feed for a patient.
_____________________________________________________
In the handout below, I have adapted these considerations to the Feed a Brain guidelines so that you can weigh the risks and benefits, and if you choose, effectively deliver foods, to this guide’s specifications, to patients who are unable to eat conventionally. Alternatively, you can purchase Feed a Brain-approved feeds and meal replacement shakes that can be fed through a gastric tube. These feeds are not as beneficial as the blenderized tube feeds outlined, but they are certainly easier to implement and are still much more beneficial than the standard hospital feed. Visit feedabrain.com/feeds to see what meal replacement and gastric feed options are available. If you are looking for optimal nutrition and have the time and energy to put into making your own blenderized feed, follow the instructions outlined in the Gastric Tube Feed Creation Instructions Handout below.
Getting the Treatment You Choose in a Hospital Setting
Cavin works with folks who have a loved one in the hospital in order to navigate a profit driven medical model and to get the best treatments, including IV vitamin therapy and real food feeds. Cavin’s track record is a 100% success rate in coaching his clients to speak with their medical team in order to get the treatments they choose, including gastric feeds, supplements, and often to also get IV nutrient injections. You can learn more about Cavin’s work throughout a medical crisis here: https://adventuresinbraininjury.com/consult
